Depression and sleep disturbances are two of the most frequently reported mental and physical health concerns. Depression affects more than 264 million people worldwide. Similarly, sleep disorders including insomnia and hypersomnia are widespread, leaving countless individuals struggling to attain restful and restorative sleep. What makes this relationship important is the frequent coexistence of these two conditions. Individuals suffering from depression frequently report difficulty sleeping, while those experiencing persistent sleep issues are more susceptible to depressive episodes.
While many people are aware that sleep and mood influence each other, the underlying mechanisms linking them are not always well understood. Understanding this connection is important, as recognising sleep not just as a symptom, but also as a contributing factor in depression can significantly improve treatment outcomes. This article will explain the link between sleep and depression by explaining how depression disrupts sleep, how poor sleep contributes to depressive symptoms, and which evidence-based treatments can effectively manage both conditions.
Understanding depression
Depression is far more than occasional sadness or transient emotional distress. It is a chronic mental health condition that significantly impairs an individual’s ability to function in daily life. The hallmark features include persistent low mood, loss of interest or pleasure in previously enjoyed activities (anhedonia), feelings of worthlessness, fatigue, and cognitive difficulties such as impaired concentration or decision-making. Physical symptoms include changes in appetite, unexplained aches, and most notably, sleep disturbances.
Depression is a heterogeneous disorder, meaning that it manifests differently across individuals. While some may experience profound lethargy and hypersomnia, others may struggle with severe insomnia and restlessness. This variability is essential to understanding how depression interacts with sleep, as the same condition can lead to drastically different sleep outcomes depending on the individual.
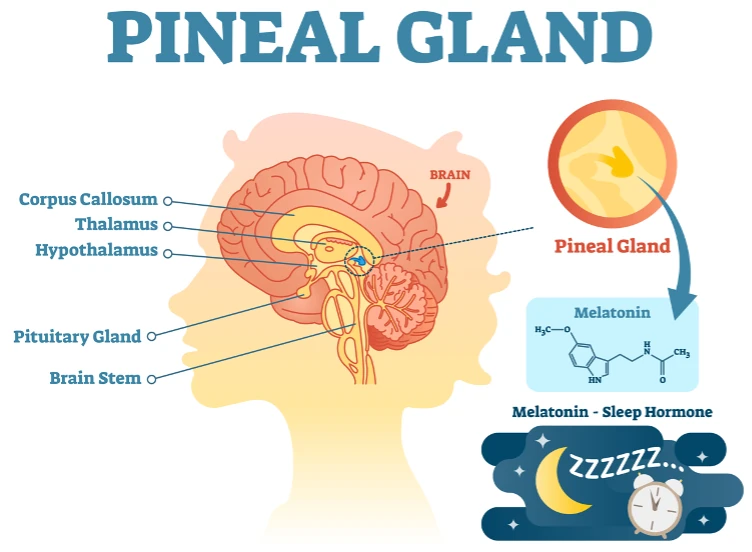
Biological factors: brain chemistry and sleep
Biologically, depression is associated with imbalances in brain neurotransmitters such as serotonin, dopamine, and norepinephrine, which play crucial roles in mood regulation and sleep-wake cycles. Serotonin is not only a mood stabiliser, but also a precursor to melatonin, the hormone that governs sleep. Disruptions in this pathway can lead to difficulty falling or staying asleep. Additionally, hyperactivity of the body’s central stress response system results in elevated cortisol levels, which can interfere with sleep initiation and maintenance.
Psychological and environmental influences
Psychologically, depression is often associated with distorted thinking patterns, such as persistent overthinking, pessimistic thoughts, and a negative self-image. These mental habits can increase anxiety and emotional tension at bedtime, making it difficult to relax and fall asleep. Furthermore, genetic predispositions and environmental stressors such as trauma, chronic illness, or major lifestyle changes contribute to the onset and maintenance of depressive symptoms, many of which disrupt regular sleep patterns.
How depression affects sleep
One of the most prevalent and troubling symptoms of depression is its impact on sleep. Individuals with depression often report insomnia, which can vary in type and severity. These include difficulty falling asleep (initial insomnia), frequent awakenings throughout the night (middle insomnia), early morning awakenings with an inability to return to sleep (terminal insomnia), and, conversely, excessive daytime sleepiness or sleeping for extended hours (hypersomnia).
Types of sleep disturbances in depression
Initial insomnia is typically associated with heightened arousal at bedtime, often due to anxiety, intrusive thoughts, or a racing mind. Middle insomnia, involving frequent disruptions in sleep continuity, may reflect the body’s heightened stress response, as individuals with depression often have increased levels of nocturnal cortisol. Terminal insomnia, characterised by waking hours earlier than desired, is particularly linked to melancholic depression, a subtype marked by severe mood disturbances and morning worsening of symptoms. Hypersomnia, although less common than insomnia, is also significant. It is more frequently seen in atypical depression and younger individuals. In these cases, patients may sleep for prolonged periods but still feel unrefreshed, pointing to poor sleep quality rather than sleep duration.
The role of brain chemistry
The brain chemistry behind sleep and depression is complicated. When serotonin levels are low, the body produces less melatonin making it harder to fall asleep. Normally, stress hormones like cortisol, epinephrine, and norepinephrine decrease at night, allowing the body to rest. But in depression, cortisol often stays high and disrupts sleep. These imbalances change how sleep cycles work. People with depression tend to get less slow-wave sleep (the most restful stage) and experience more intense REM sleep, leaving them feeling exhausted even after a full night in bed. This broken sleep pattern worsens fatigue and mood, creating a tough cycle to break.
Emotional and cognitive disruptions to sleep
Beyond the biological aspects, emotional and cognitive features of depression play an important role in sleep disturbance. Rumination and self-critical thoughts become particularly pronounced at night. This mental activity delays sleep onset and contributes to fragmented sleep. Negative emotions, such as guilt or hopelessness, can create a state of psychological hyperactivity, and disrupt the relaxation necessary for restful sleep. Together, these cognitive and emotional challenges contribute to insomnia, creating a cyclical relationship between depression and poor sleep.
How sleep issues can worsen depression
While depression can disturb sleep, sleep issues can also significantly exacerbate depressive symptoms. Chronic sleep disturbances are not only a symptom but also a predictor of depression. Individuals suffering from insomnia are at a substantially higher risk of developing depression, and those with existing depressive disorders often experience more severe symptoms when sleep is compromised.
Biological effects of poor sleep on depression
From a biological standpoint, inadequate sleep impairs the brain’s ability to regulate emotions effectively. Sleep deprivation diminishes activity in the prefrontal cortex the brain region responsible for executive function and emotional control while increasing reactivity in the amygdala, the center of emotional processing. This imbalance results in increased emotional volatility, negative thinking, and impaired coping mechanisms, all of which worsen the depressive state.
Psychological and behavioural impact
Psychologically, sleep deprivation contributes to a decline in motivation, concentration, and energy levels, which can mimic and amplify core symptoms of depression. Poor sleep disrupts daily routines and social engagement, increasing feelings of isolation and hopelessness. Moreover, the frustration and helplessness caused by persistent insomnia can lead to further rumination and self-blame, reinforcing depressive thoughts.
The vicious cycle and risks of poor sleep
A particularly concerning aspect of the relationship between sleep and depression is the emergence of a vicious cycle. Poor sleep exacerbates mood disturbances, which in turn make it more difficult to fall or stay asleep. Furthermore, sleep disturbances are closely linked to suicidal ideation and behaviour. Individuals with both depression and insomnia are at a higher risk for suicidal thoughts and actions compared to those with depression alone, highlighting the urgent need for early intervention.
This bidirectional relationship emphasises the importance of treating sleep disorders not as secondary to depression but as integral components of the condition. Improvements in sleep have been consistently associated with better treatment outcomes, reduced symptom severity, and lower relapse rates in depression. Thus, breaking the cycle of poor sleep and low mood can be a powerful step toward recovery.
The role of circadian rhythms in depression and sleep
Circadian rhythms (the body’s internal clock) govern the sleep-wake cycle and many other physiological functions. These rhythms are regulated by the suprachiasmatic nucleus in the brain and are highly responsive to environmental cues like light and temperature. Disruptions to this system, such as those caused by shift work, jet lag, or irregular sleep schedules, have been linked to both sleep disorders and mood disturbances. In individuals with depression, circadian rhythm disruptions are particularly common and often manifest as misaligned sleep timing or irregular daily patterns.
People with depression frequently experience delayed sleep-wake phase disorder, where their natural tendency is to fall asleep and wake up later than socially acceptable hours. This misalignment can lead to chronic sleep deprivation, as societal demands force early rising despite insufficient rest. Over time, this leads to cumulative fatigue and emotional strain, worsening depressive symptoms and impairing daytime functioning.
Bright light therapy, morning exposure to sunlight, and structured daily routines have been shown to help realign circadian rhythms and improve both mood and sleep. These interventions target the underlying biological clock rather than just the symptoms, offering a non-pharmacological way to manage depression and sleep disturbances. When implemented consistently, they can contribute to more stable sleep patterns and improved emotional regulation.
Circadian misalignment can influence the timing of hormone release, including melatonin and cortisol, in ways that exacerbate mood symptoms. In depressed individuals, abnormal timing of cortisol secretion such as elevated levels in the evening can impair the body’s ability to relax, contributing to both sleep onset difficulties and emotional instability. A broad range of body functions such as appetite, sleep, activity and cortisol levels are controlled by the circadian clock. Furthermore, disruption of circadian-regulated processes such as body temperature and metabolic function may also play a role in the persistence of both sleep and mood symptoms.
Cognitive and behavioural factors beyond the nighttime
While bedtime rumination and hyperarousal are often discussed, the cognitive and behavioural effects of depression on sleep extend well beyond nighttime hours. Daytime behaviours such as excessive daytime sleepiness, inactivity, or irregular mealtimes can inadvertently disrupt the body’s natural sleep pressure, reducing the drive to sleep at night. Over time, these behaviours create a mismatch between sleep needs and actual sleep ability, making it harder to maintain healthy sleep routines.
Furthermore, individuals with depression often develop negative sleep-related beliefs like “I’ll never be able to sleep” or “If I don’t sleep, my day will be a disaster.” These thoughts can increase sleep anxiety and heighten pre-sleep arousal. Such anticipatory anxiety often triggers insomnia, highlighting the importance of addressing these thought patterns through targeted cognitive behavioural therapy for insomnia (CBTi).
Low motivation and executive dysfunction are common in depression, making it difficult for individuals to consistently engage in habits that promote good sleep. Without support, it can be challenging to maintain structure or follow through with behavioural recommendations like reducing caffeine or sticking to a bedtime routine. Addressing these cognitive and behavioural challenges through therapy or coaching can support long-term improvements in both mood and sleep.
Treatment Options: addressing depression and sleep issues
To effectively treat depression and sleep problems, it’s important to work on both at the same time. Treating one condition without attending to the other often leads to suboptimal outcomes and increases the risk of relapse. Fortunately, various therapeutic approaches have been developed and refined to target both mood and sleep disturbances simultaneously.
Cognitive Behavioural Therapy (CBT and CBT-I)
Cognitive Behavioural Therapy (CBT) remains the gold standard for depression and is particularly effective when tailored for insomnia. Cognitive behavioural therapy for insomnia (CBT-I) focuses on identifying and modifying unhelpful beliefs about sleep, establishing consistent sleep-wake schedules, and incorporating relaxation techniques. It also involves stimulus control therapy, which aims to strengthen the bed-sleep connection by limiting non-sleep activities in bed, such as reading or screen time. CBT-I significantly improves sleep quality while also reducing depressive symptoms, particularly when used as part of a comprehensive mental health treatment plan.
Pharmacological interventions
Pharmacological interventions can also be beneficial. Certain antidepressants, particularly those with sedative properties such as mirtazapine or trazodone, can aid sleep while addressing mood symptoms. However, not all antidepressants are sleep-promoting. Fluoxetine or sertraline may initially disrupt sleep, though they often stabilise sleep patterns over time. Medication decisions must be made collaboratively with a healthcare provider, taking into account individual symptoms, side effect profiles, and the potential for dependency on sleep aids such as benzodiazepines or over-the-counter medications.
Lifestyle changes and sleep hygiene
In addition to therapy and medication, lifestyle and behavioural changes play an important role in managing both depression and sleep disturbances. Establishing a regular sleep routine, avoiding caffeine and alcohol in the hours before bedtime, and engaging in regular physical activity are foundational to good sleep hygiene. Techniques such as mindfulness meditation, progressive muscle relaxation, and guided imagery can also reduce arousal and facilitate sleep onset.
The role of screen time and individualised treatment
Limiting screen time, especially in the evening hours is another essential strategy. Blue light emitted by smartphones, tablets, and computers suppresses melatonin production, delaying sleep onset. Replacing screen-based activities with calming pre-sleep routines can make a difference. Each patient presents with a unique combination of symptoms, preferences, and challenges so treatment must be individualised. A personalised, holistic treatment plan developed in consultation with a mental health or sleep specialist is often the most effective approach. By addressing both the psychological and physiological components of depression and sleep disruption, individuals are better positioned to achieve lasting improvement.
When to seek help
Recognising when to seek professional help is crucial. While occasional sleep disturbances or transient low moods are common, persistent issues demand clinical attention. You should seek professional help if you experience persistent sleep problems like insomnia or excessive sleeping, along with unrelenting fatigue, loss of interest in daily activities, difficulty concentrating, or prolonged feelings of hopelessness that interfere with your quality of life. These symptoms often indicate that both your sleep and mood need clinical attention, as leaving them untreated may allow the cycle between poor sleep and depression to continue worsening.
Both depression and sleep disorders are highly treatable, particularly when they are addressed together. A qualified professional can conduct a comprehensive assessment, rule out underlying medical issues, and formulate a treatment plan tailored to your specific needs.
Combating depression and sleep issues
The connection between depression and sleep is bidirectional. Depression can severely disrupt sleep patterns, and in turn, poor sleep can intensify and prolong depressive symptoms. Understanding this relationship is essential for effective treatment and improved quality of life. Rather than treating sleep issues and mood disorders in isolation, an integrated approach offers the best chance for recovery. With the right combination of therapeutic strategies, lifestyle changes, and professional support, individuals can regain restorative sleep and improve their mental wellbeing.
If you or someone you care about is struggling with depression and sleep difficulties, it’s time to take the next step toward recovery. Dr Dipesh Mistry specialises in diagnosing and treating sleep disorders, offering compassionate, tailored care that addresses the full spectrum of your mental and physical health needs. Contact us today to schedule an initial consultation, request more information, or begin your journey toward better sleep and brighter days.