Sleep disorders have become increasingly prevalent, affecting millions of individuals worldwide. They have a profound impact on mental health and overall well-being. Insomnia is one of the most prevalent sleep disorders, often coexisting with other conditions such as Attention-Deficit Hyperactivity Disorder (ADHD). ADHD is characterised by persistent patterns of inattention, hyperactivity, and impulsivity and affects approximately 2.5 – 6.7 % of adults globally. These symptoms can make it challenging for individuals to focus, control their impulses, and manage their daily responsibilities effectively.
Insomnia is defined as persistent difficulty with sleep initiation, maintenance, and early morning awakening despite adequate opportunity for sleep. The relationship between these two conditions is complex and often leads to a cycle of disruptions that can significantly impact an individual’s quality of life. This article will discuss the relationship between ADHD and insomnia, with a focus on their impact on daily life.
The complex relationship between ADHD and insomnia
The relationship between ADHD and insomnia is complex, with several factors contributing to their coexistence. A hyperactive mind is the characteristic of ADHD, which can make it challenging to quieten the mind and transition into sleep. This overactivity often extends to emotional regulation, leading to heightened stress or frustration when trying to fall asleep. Additionally, irregular sleep patterns and difficulty adhering to bedtime routines are common in individuals with ADHD, further complicating sleep initiation.
Anxiety is a common companion to ADHD, which further exacerbates insomnia. Many individuals with ADHD experience anxiety related to work or academic responsibilities, social anxiety related to interpersonal challenges, or general anxiety about managing daily tasks. These anxiety patterns can create a cycle of worry that becomes particularly pronounced during the quiet evening hours, making it difficult to achieve restful sleep.
The role of ADHD medications in sleep disturbances cannot be overlooked. While these medications are essential for managing ADHD symptoms, some stimulant medications may have side effects that impact sleep patterns. The timing of medication doses, duration of action, and individual sensitivity can all influence sleep quality. For example, long-acting stimulants taken too late in the day may interfere with natural sleep onset, while wearing off too early might lead to evening symptom rebound that disrupts bedtime routines. It must be noted that there are conflicting studies and hence the effect of stimulants may vary between individuals and that is very likely the case.
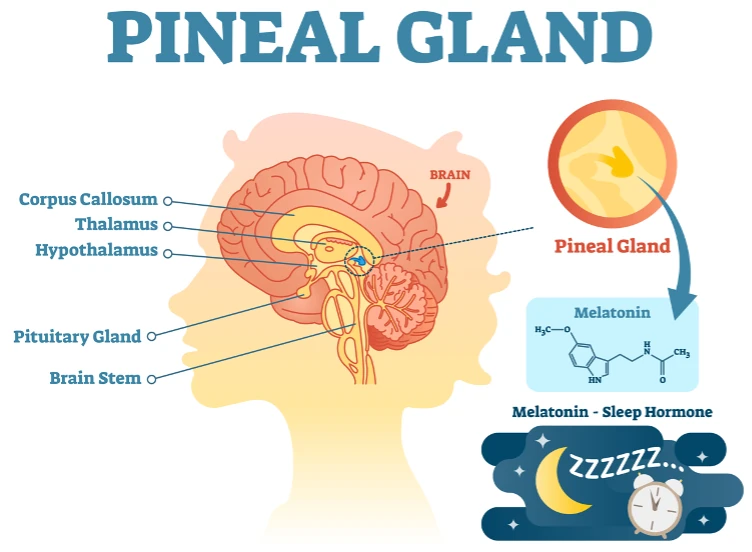
The relationship between ADHD and sleep is bidirectional, as sleep deprivation can significantly exacerbate ADHD symptoms. Poor sleep quality or insufficient sleep duration can impair cognitive function, increase irritability and impulsivity, and worsen emotional dysregulation. This creates a challenging cycle where ADHD symptoms interfere with sleep, and poor sleep, in turn, intensifies ADHD symptoms. Additionally, differences in melatonin production and timing have been observed in individuals with ADHD, potentially contributing to delayed sleep phase syndrome and other circadian rhythm disruptions.
How do ADHD-related sleep problems affect daily life?
The impact of sleep problems on individuals with ADHD extends far beyond nighttime discomfort, affecting virtually every aspect of daily functioning. Understanding these wide-ranging effects is crucial for developing comprehensive treatment approaches and support strategies.
Cognitive function
The combination of ADHD and insomnia significantly affects attention, concentration, and executive functioning. Sleep deprivation can impair working memory, decision-making abilities, and problem-solving skills, making it even more difficult for individuals with ADHD to manage their typical symptoms effectively. Sleep deprivation can reduce cognitive processing, particularly affecting tasks requiring sustained attention and complex problem-solving. Executive functions, including planning, organisation, and time management, are particularly vulnerable to sleep disruption. Research has shown that even one night of poor sleep can reduce executive function performance, with cumulative effects building over time with chronic sleep problems.
Academic and work performance
Sleep deprivation negatively impacts students’ academic performance. Students with ADHD and insomnia may find it increasingly difficult to focus during lectures, complete assignments on time, or retain information while studying. In the workplace, sleep-deprived individuals might experience decreased productivity, increased error rates, and difficulty meeting deadlines. Moreover, the combination of ADHD and sleep problems can affect workplace safety, particularly in jobs requiring the operation of machinery or careful attention to detail. Sleep deprivation can impair reaction times and decision-making capabilities to a degree comparable to alcohol intoxication.
Social and interpersonal relationships
Sleep problems can significantly affect emotional regulation, leading to irritability, mood swings, and difficulty managing emotions. This lack of control over emotions can make it harder to handle stressful situations, compounding feelings of frustration and overwhelm. As emotional resilience diminishes, individuals may also struggle to recover quickly from negative experiences, prolonging interpersonal conflicts.
These emotional challenges can strain relationships with family, friends, and colleagues, as individuals may react more impulsively or be less patient in social interactions. Over time, these issues can create tension in both personal and professional relationships, as people may feel frustrated or misunderstood. In families, the inability to manage emotions can lead to conflicts, while in the workplace, it may hinder collaboration and productivity.
Physical health
ADHD causes insomnia, which increases the risk of developing type 2 diabetes and contributes to obesity by disrupting hormones that regulate appetite and metabolism. Chronic sleep deprivation can also elevate stress hormone levels, further exacerbating metabolic imbalances. Poor sleep may lead to increased cravings for unhealthy foods, compounding weight management difficulties. Additionally, chronic sleep problems can weaken the immune system, lower pain thresholds, and increase inflammation which exacerbates chronic pain conditions.
Over time, the cumulative effects of poor sleep can lead to greater physical exhaustion, reducing the body’s ability to recover and heal. These health challenges can complicate the management of ADHD symptoms, potentially creating a cascade effect that negatively impacts overall health and well-being.
Mental health
The combination of ADHD and insomnia can significantly increase the risk of developing various mental health conditions. Individuals with both ADHD and sleep problems face an increased risk of developing depressive disorder, often compounded by feelings of frustration and hopelessness over their sleep challenges. Sleep disruption can also impair emotional regulation, making it harder to cope with daily stressors.
Additionally, sleep disruption can worsen anxiety symptoms and create new patterns of anxiety. Over time, the cumulative effects of poor sleep and untreated ADHD can lead to burnout, further impacting mental health stability. In some cases, individuals may resort to alcohol or other substances in an attempt to manage their sleep difficulties, further complicating the situation. This creates a complex web of interconnected symptoms that can be challenging to address effectively without professional intervention.
Diagnostic considerations
Accurate diagnosis of both ADHD and insomnia requires a thorough evaluation that considers the full spectrum of symptoms and their potential interactions. Healthcare providers must assess sleep patterns, ADHD symptoms, and any other contributing factors to create an effective treatment plan. The diagnostic process should include a detailed sleep history, sleep diary analysis, and a comprehensive ADHD symptom assessment. It should also involve evaluating co-existing medical conditions, reviewing current medications and substances, and assessing lifestyle factors that may be affecting sleep. Additionally, considering circadian rhythm patterns and screening for other sleep disorders is essential to ensure a comprehensive understanding of the individual’s health.
Collaboration between sleep specialists and mental health professionals specialising in ADHD can provide valuable insights and lead to more accurate diagnoses. Their combined expertise allows a deeper understanding of how ADHD symptoms and sleep disturbances interact. This multidisciplinary approach ensures that both conditions are properly identified and improves outcomes for people with ADHD. By working together, healthcare providers can develop a tailored treatment plan that improves sleep quality and helps to manage ADHD symptoms effectively.
Treatment approaches
Non-pharmacological interventions, such as cognitive-behavioural therapy for insomnia (CBT-I) and cognitive-behavioural therapy for ADHD (CBT-ADHD), offer effective treatment options for both conditions. CBT-I helps individuals to develop healthy sleep habits by addressing cognitive and behavioural factors contributing to insomnia. This therapy focuses on techniques like sleep hygiene education, stimulus control, and sleep restriction, which help to regulate sleep patterns and improve sleep quality.
By targeting the underlying causes of insomnia, CBT-I empowers individuals to overcome sleep difficulties without relying on medication. Similarly, CBT-ADHD helps individuals develop coping strategies for managing ADHD symptoms. It emphasises the development of organisation and time management skills and cognitive restructuring to challenge negative thought patterns and build self-regulation. Together, these therapies provide a structured approach to managing both insomnia and ADHD, improving overall functioning and quality of life.
The integration of stress management techniques can significantly benefit individuals with ADHD and insomnia. Mindfulness practices, such as regular meditation, body scan exercises, and mindful breathing, can reduce stress and improve focus. Engaging in activities like exercise and yoga can promote overall well-being. Environmental modifications, such as creating organised living and working spaces, reducing distractions, and ensuring proper lighting and temperature control, can further enhance focus and improve sleep quality.
Medication management for concurrent ADHD and insomnia requires careful consideration. For ADHD medications, optimising the timing of stimulant medications is essential to avoid interference with natural sleep cycles. Monitoring the impact of medicines on sleep patterns and adjusting doses to minimise sleep disturbances is also important. Healthcare providers may also explore alternative formulations or non-stimulant options if sleep issues persist. Melatonin supplementation can help to address insomnia by regulating circadian rhythms and promoting sleep onset. However, it’s crucial to assess potential interactions with ADHD medications and develop medication tapering plans to avoid dependency or side effects. Regular follow-ups with a healthcare provider ensure that the treatment plan remains effective and adaptable to changing needs.
ADHD and trouble sleeping
The connection between ADHD and insomnia represents a complex interaction of neurological, behavioural, and environmental factors. Understanding this relationship is crucial for developing effective treatment strategies that address both conditions simultaneously. While the challenges of managing both ADHD and sleep problems can seem daunting, numerous evidence-based interventions are available to help individuals achieve better sleep and improved daily functioning.
Success in managing these conditions often requires a comprehensive approach that combines professional support, lifestyle modifications, and appropriate medical interventions. Incorporating regular follow-ups ensures that treatment plans remain effective and are adjusted to meet changing needs. With proper diagnosis and treatment, individuals can develop effective strategies for managing both their ADHD symptoms and sleep difficulties, leading to improved quality of life and better overall health outcomes.
If you’re struggling with ADHD and sleep problems, consider scheduling consultations with mental healthcare professionals who specialise in each of these conditions. An ADHD specialist can provide a thorough evaluation and develop a personalised treatment plan that addresses your specific needs and concerns. The journey to better sleep and ADHD management is ongoing, but with the right support, strategies, and commitment, significant improvements are possible. Dr Dipesh Mistry is a leading sleep specialist in the UK who helps people with their sleep problems. Schedule an appointment to take the first step towards achieving a high-quality, restful sleep.
Summary
Here is a quick summary to help you digest the key points:
- ADHD and insomnia are closely linked, with ADHD causing sleep difficulties due to hyperactivity, anxiety, and the side effects of medication.
- Sleep problems affect cognitive abilities, work and academic performance, emotional regulation, and overall physical health.
- Treatment includes cognitive-behavioural therapy for insomnia (CBT-I) and ADHD (CBT-ADHD), alongside stress management techniques and environmental adjustments.
- Medication management involves adjusting ADHD medication timing and doses and the use of supplements like melatonin while carefully monitoring for any potential interactions.
- If you are having trouble sleeping, it may be wise to consult a sleep specialist to rule out any medical causes.