Insomnia affects 1 in 3 people in the UK, with a higher prevalence in the elderly. Insomnia is a condition that can affect anyone, but has been noticed to affect women more than men. A combination of multiple factors could make women more susceptible to developing insomnia compared to men, and it is essential to know about these potential causes so that you can address your sleeping problems and overcome your insomnia.
What is insomnia?
Insomnia is a common sleeping disorder that makes it hard to fall asleep or stay asleep at night. This often results in individuals feeling exhausted, sleepy and struggling to function as they normally would the following day. Individuals will often notice that this leads to disruptions in their daily routines, significantly impacting many aspects of their life.
Learn more about what Insomnia is: What is insomnia and can it be cured?
Is insomnia more common in women?
Over time, research has shown that insomnia is considerably more common in women than in men. These higher rates of insomnia in females have been noticed in many studies. According to the National Institute of Health and Care Excellence and a 2019 study, the prevalence of insomnia is at least 1.5-2 times higher in females than males. It has also been noted that insomnia can occur at any age but is most common in older adults. Furthermore, insomnia is more common in those with other comorbid conditions such as chronic obstructive pulmonary disease (COPD), heart failure, chronic pain, and psychiatric conditions – around half of all people with diagnosed insomnia also have a comorbid psychiatric condition.
Researchers believe that insomnia is more common in women than men due to a combination of factors such as gender differences and other independent variables. These sex-based differences in sleep are related to the biological variation between males and females, including hormone production. Gender-based differences may be driven by social and cultural differences affecting sleep.
In addition to this, predispositions to physical and mental health issues may also contribute to the higher rates of insomnia among females. Overall, there are a lot of possible confounding factors that may be contributing to why women are more likely to have insomnia.
Why is insomnia more common in women?
Whilst the consensus is not clear on the exact cause for the higher rates of insomnia amongst women, studies indicate a clear difference between the two genders. Below are some of the common reasons thought to be the cause of a higher incidence of insomnia among women:
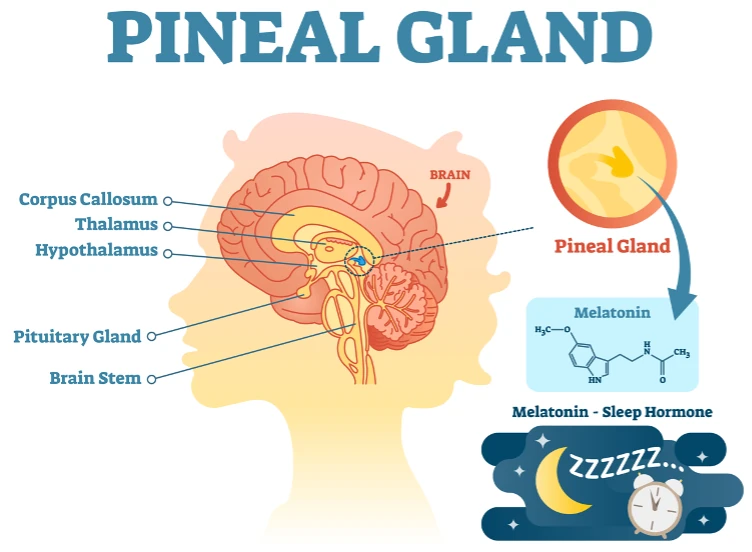
Premenstrual syndrome (PMS): Women with PMS are twice as likely to experience insomnia before and during their period. It is thought that hormonal changes before and during menstruation may affect body temperature and melatonin production. These changing hormone levels may cause sleeping difficulties and more disturbed sleep.
Premenstrual dysphoric disorder (PMDD): 70% of women with PMDD have insomnia-like problems before their period, and over 80% describe feeling tired.
Pregnancy: Women may sleep less deeply during pregnancy, causing increased wakenings at night and fragmented sleep. Several factors could affect your sleep during pregnancy and may start as early as the first trimester when hormonal changes occur. Sleep problems become more common in the third trimester as the body changes and fetal growth continues. Common causes of insomnia during pregnancy include: nausea, hormonal changes, increased metabolism and heart rate, snoring, physical discomfort, frequent nighttime bathroom trips, heartburn and anxiety.
Perimenopause and menopause: This can cause hot flashes and night sweats, thus affecting your sleep. During this stage of life, women may also develop other sleeping disorders, which may cause insomnia-like symptoms such as sleep apnoea.
Medication: Some drugs contain caffeine, which is a stimulant and thus keeps you awake at night.
Mental health: Mental health disorders (particularly depression, anxiety and stress) can cause symptoms like racing thoughts and forms of stress, leading to individuals being kept awake at night. It is commonly noted that other psychiatric disorders are often found with insomnia. People with insomnia are 10 times more likely to have depression and 17 times more likely to have anxiety. Researchers aren’t sure if mental health conditions lead to insomnia or if insomnia leads to mental health conditions. It is likely that the relationship between insomnia and mental health conditions is bidirectional. It is widely known and accepted that a lack of sleep may cause a worsening of mental health conditions.
Fibromyalgia: The pain experienced from fibromyalgia can make it difficult to fall asleep and stay asleep.
Other causes of insomnia include urinary problems, sleep apnoea, parasomnias and restless legs syndrome. If you suspect another sleep condition may be causing or worsening your insomnia, please contact your local GP or sleep specialist for the appropriate advice.
The role of hormones in insomnia
Hormones are the body’s chemical messengers and play a vital role in the body’s functioning. Hormones can directly or indirectly affect our sleep. It is widely accepted that hormonal differences are likely to be an underlying drive of distinct sleep patterns in women, including higher rates of insomnia. Hormone production, however, is dynamic and changes as you get older, and during the monthly menstrual cycle.
Oestrogen and progesterone are the two primary hormones that play a role in insomnia and women’s health. Oestrogen regulates the menstrual cycle, pregnancy, bone strength and other functions for women. Progesterone plays a key role during pregnancy and maintaining it.
Studies show that an elevated risk of insomnia is associated with the onset of menstruation. The exact reason for this is unknown, but it may be tied to oestrogen, progesterone, and other hormones influencing our sleep cycle. In addition to this, evidence suggests that girls during puberty are more susceptible to depression, a mental health condition often found with sleeping disorders including insomnia.
Changes in hormone production drive the phases of menstruation. Rising and falling levels of oestrogen and progesterone can induce physical and emotional changes over each month. Women with conditions such as PMS or PMDD often report insomnia-like symptoms and often experience poorer sleep quality.
Women also experience significant changes in hormone production during pregnancy, which can cause fatigue, morning sickness, weight gain and a range of other physical and emotional changes. These ongoing hormonal fluctuations during pregnancy can disrupt the sleep-wake cycle, and many find their sleeping problems significantly worsen during the third trimester.
What’s the best treatment for insomnia in women?
Unfortunately, there are currently no evidence-based treatments that are focused specifically on insomnia occurring in women. We recommend contacting your local GP or sleep specialist for specific advice tailored to your needs.
Treatments that you could consider for treating insomnia include:
- Trying breathing techniques to help you relax before sleep
- Considering your sleep environment, e.g. temperature, bedding and more
- Putting your phone away before bed and avoiding blue light
- Listening to calming music before bed as a way of relaxing
- Reading a book to ease you into sleep
- Trying items such as weighted blankets to provide comfort whilst asleep
If these remedies do not work, we recommend trying other solutions here.
If you have tried the above interventions and are still struggling with your sleep, you may wish to consider a consultation with a sleep specialist for a comprehensive assessment of your sleeping difficulties.
When to see a specialist sleep doctor?
Insomnia is a silent yet deadly killer of our sleep. Most people will need between 7 to 9 hours of sleep every night to be refreshed and energised for the next day. Chronic insufficient sleep can be associated with other health conditions and an overall decrease in our performance. Early assessment by your GP or a sleep specialist can be helpful for avoiding your sleeping difficulties from escalating.
We have had the chance to help many women tackle insomnia through CBTi and other methods. This journey starts with a consultation to allow us to assess the nature and severity of your insomnia, and identify any causes.
We have had the pleasure of working with Ingeborg Van Lotringen and helping her take control of her sleep through my 5-week CBTi course. You can read more about her experience here and how we helped her.
We hope you have found this article helpful in understanding why women are often more prone to insomnia than men, and how you could improve your sleep quality. If you have any further queries about insomnia in women, please do not hesitate to contact us.